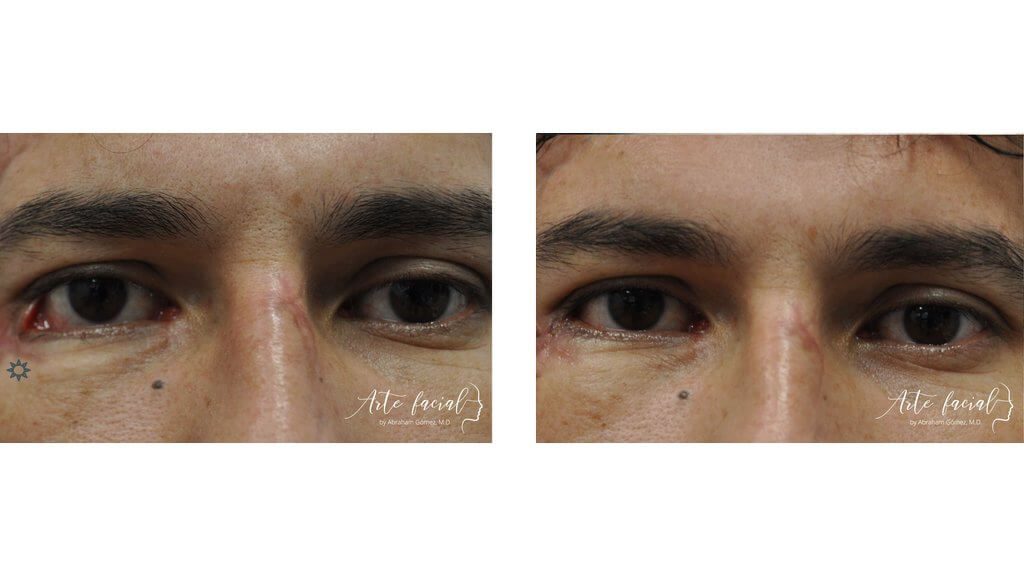
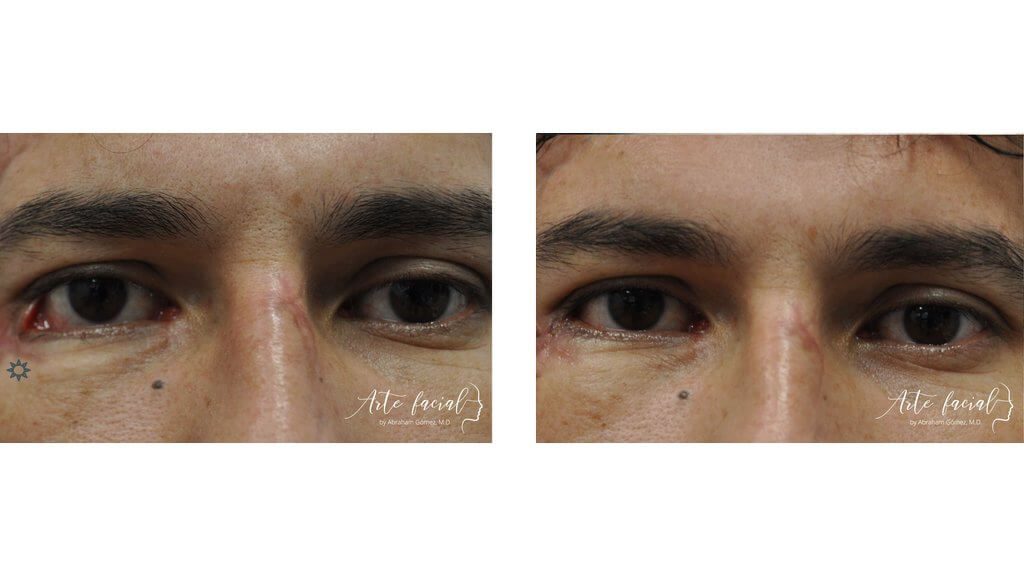
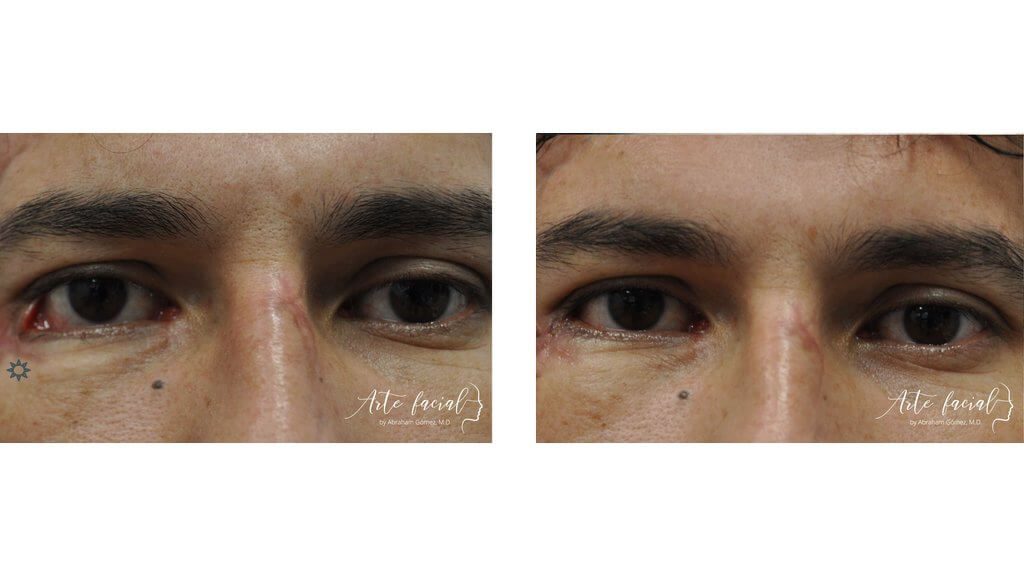
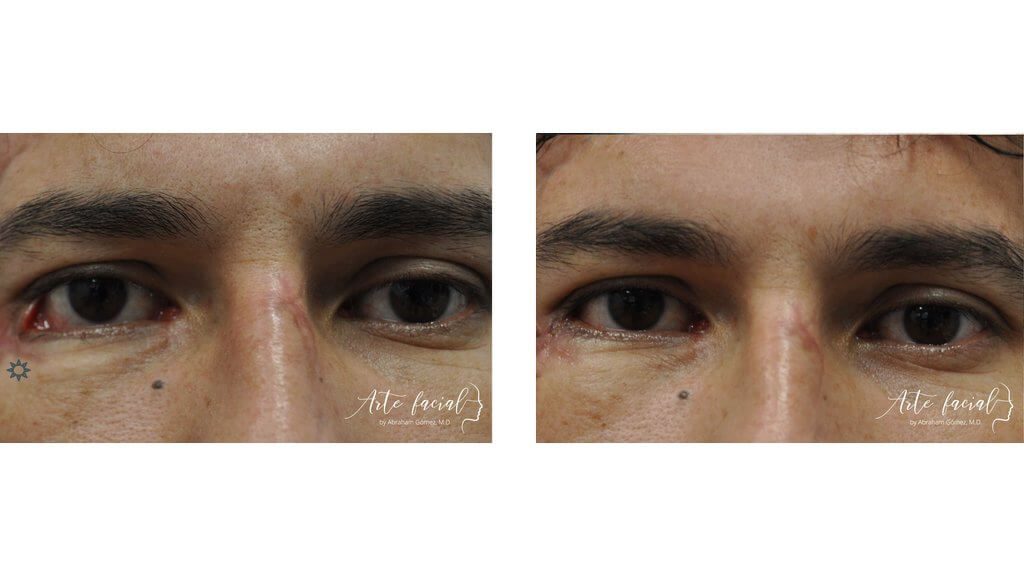
Before
After

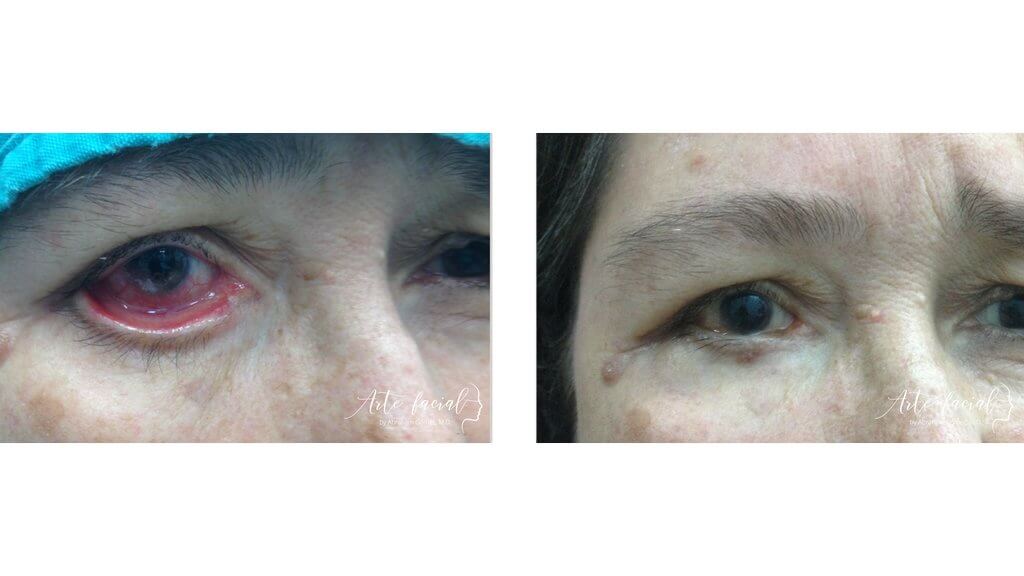
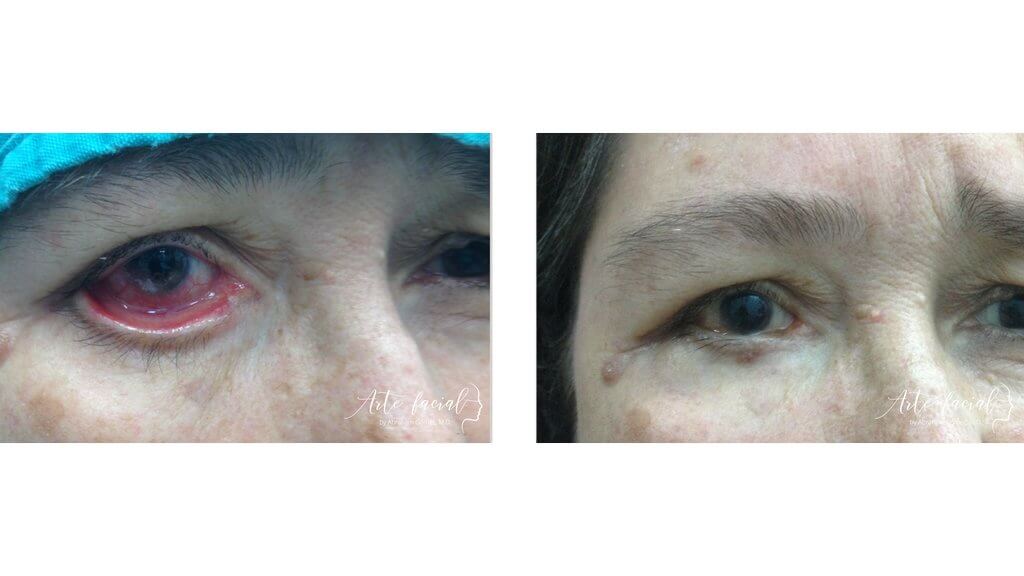
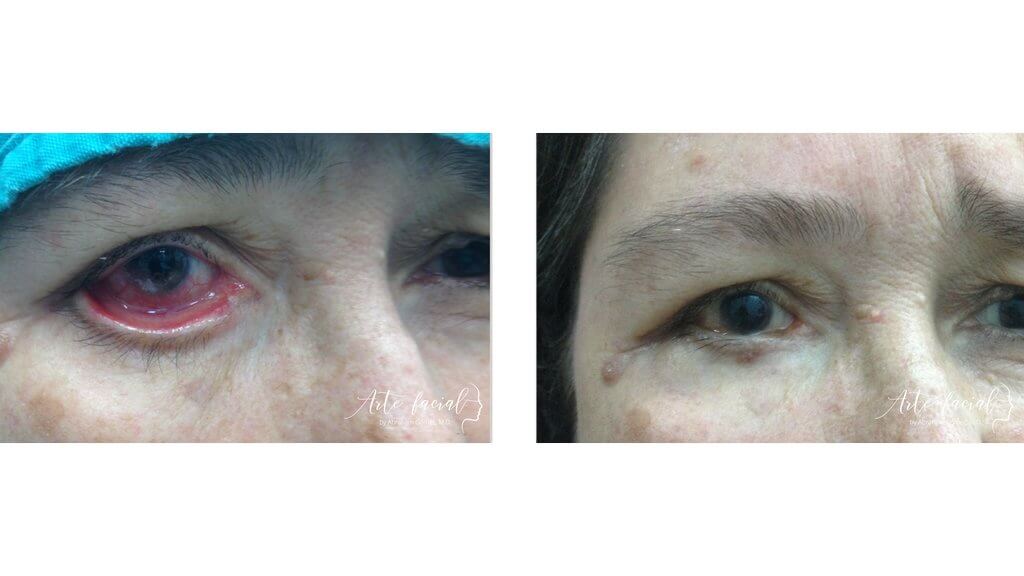
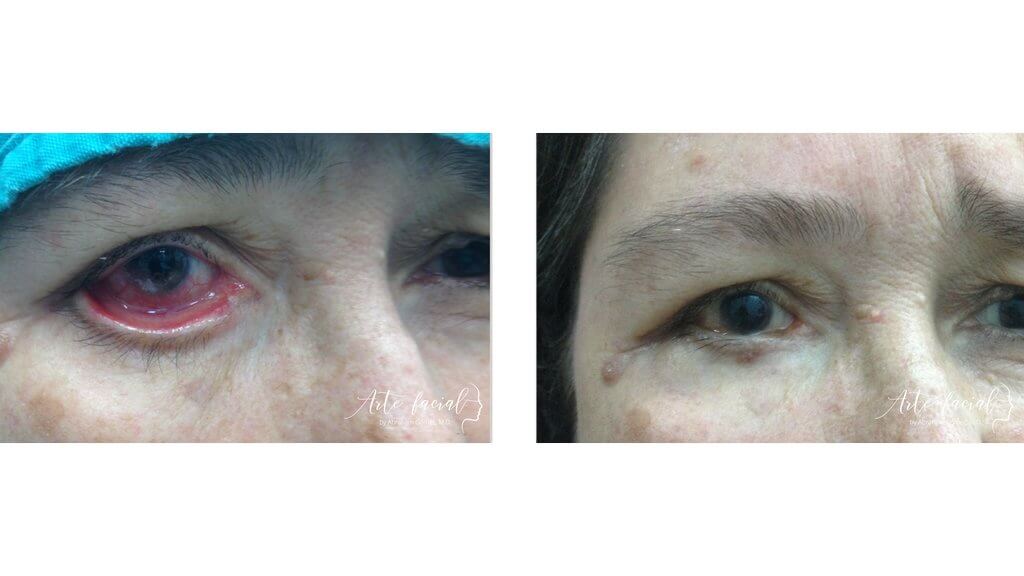
Functional & reconstructive (3)
Functional & reconstructive (4)
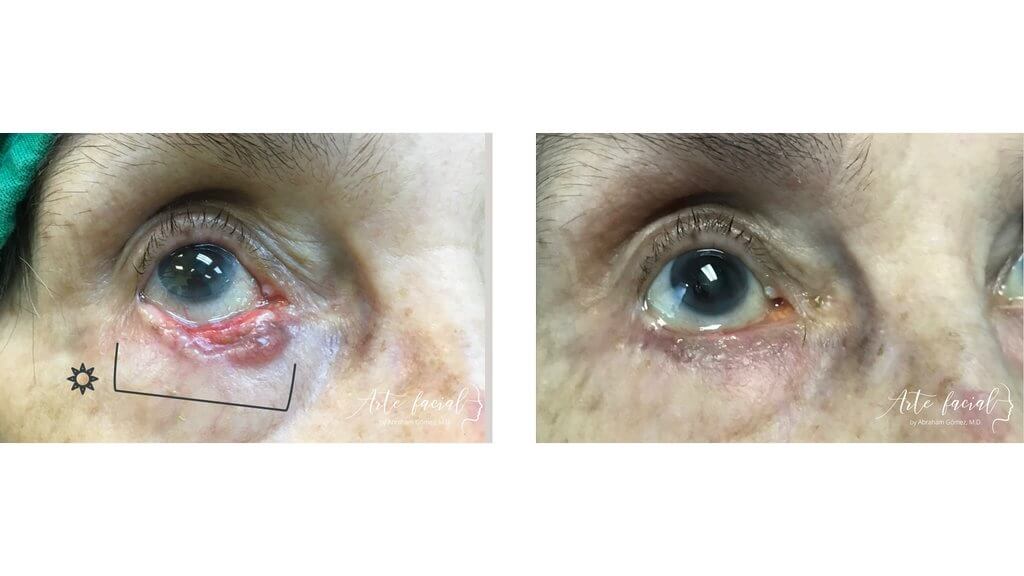
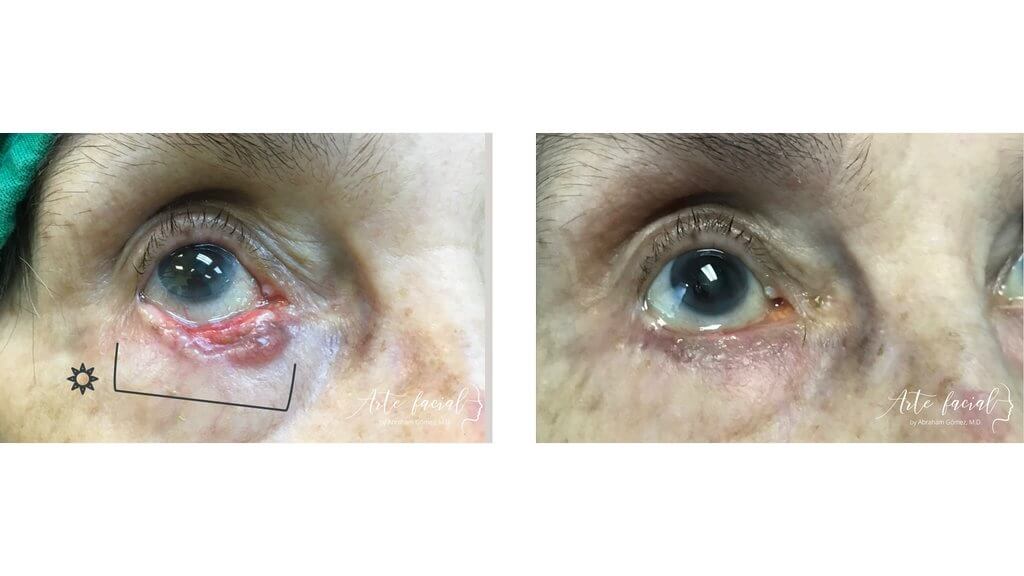
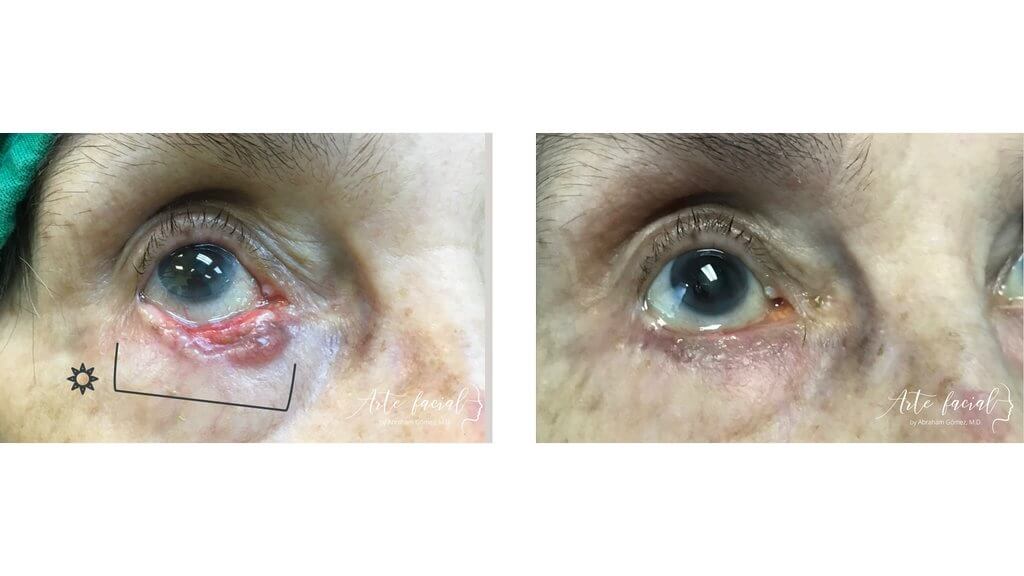
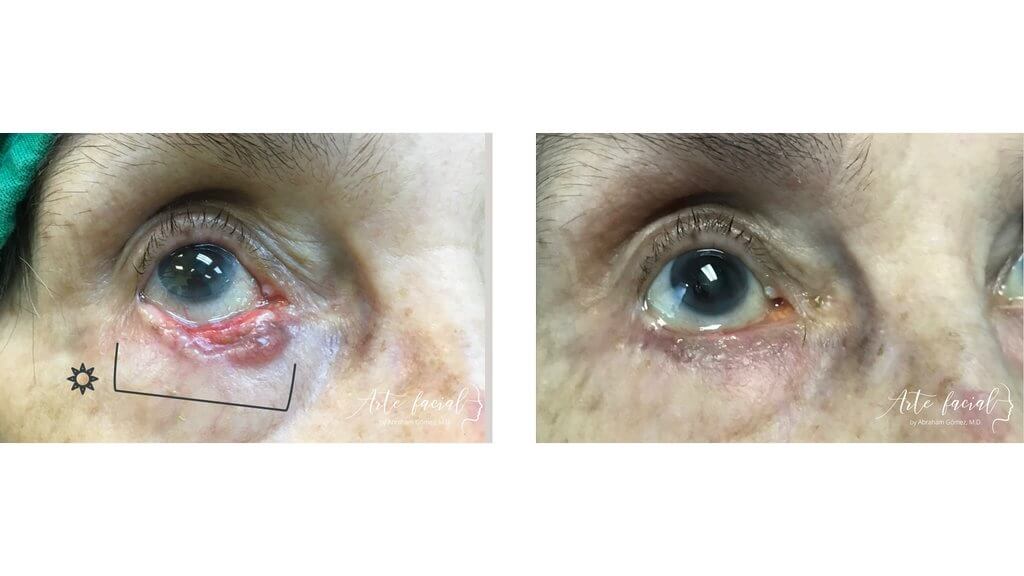
Functional & reconstructive (5)
Functional & reconstructive (6)
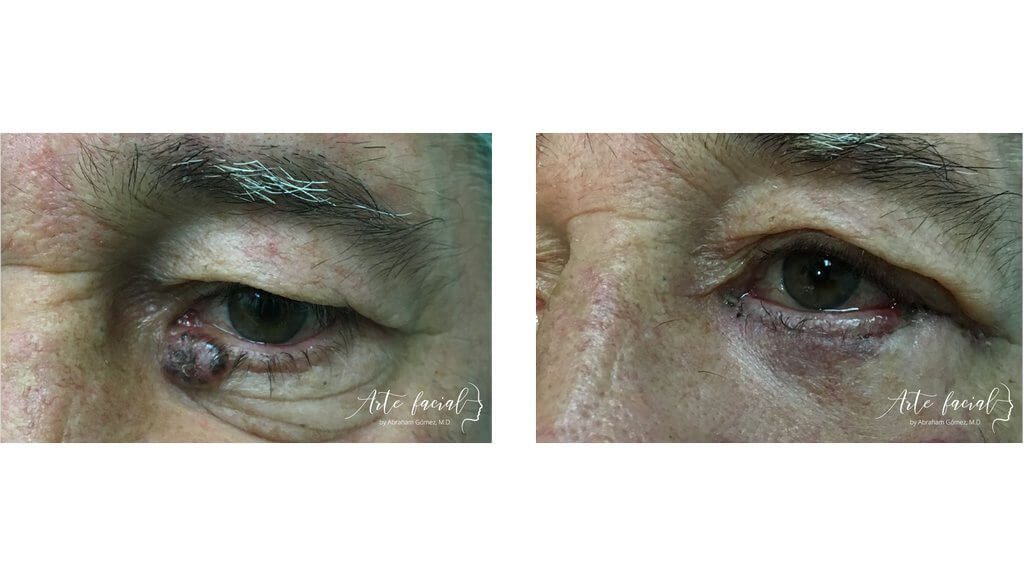
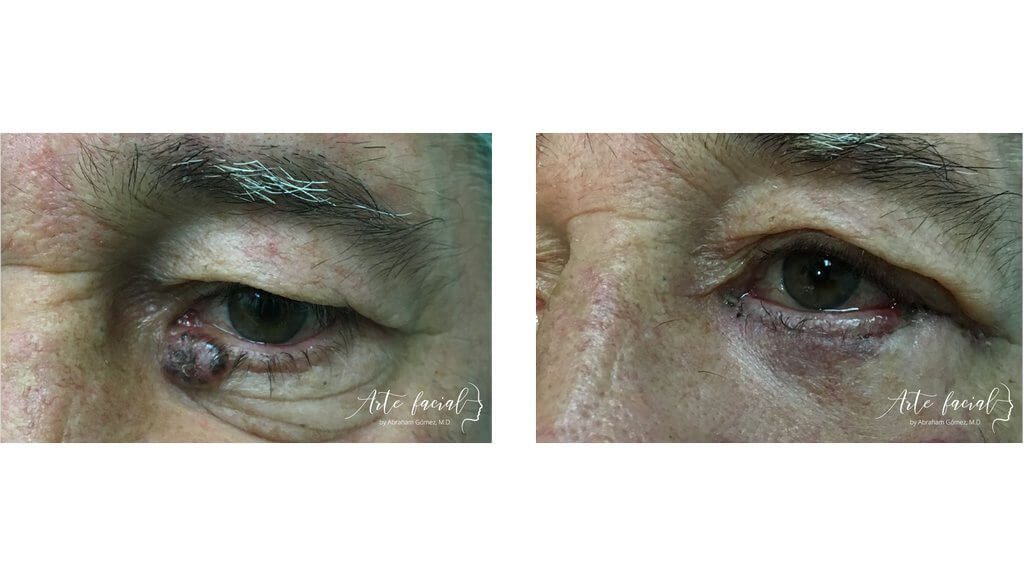
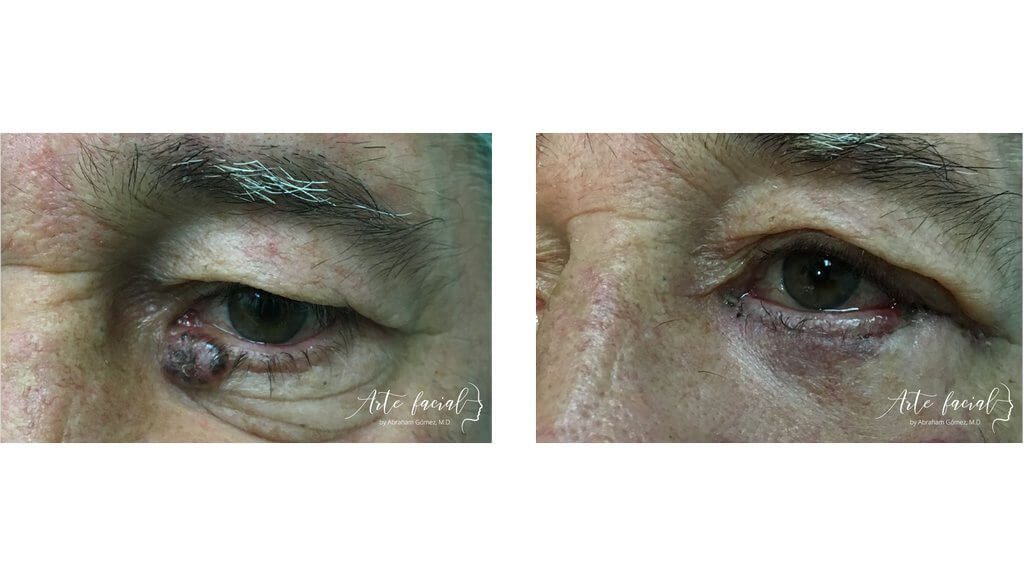
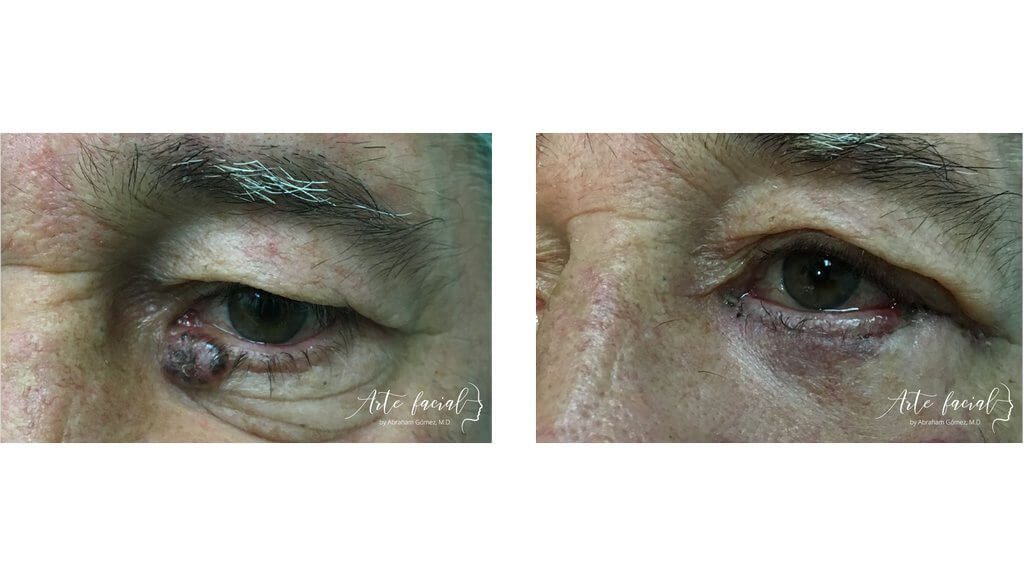
Functional & reconstructive (7)

Facial paralysis is a common medical condition in which the nerve responsible for carrying signals from the brain to the facial muscles is temporarily or permanently damaged. This typically results in the weakening of the muscles responsible for blinking. Without the proper function of these muscles, the eyelids will not close properly causing the surface of the eye to become dry; this condition is known as lagophthalmos. The upper eyelid can open normally but will not close completely, especially during sleeping hours. If untreated, the eye will become severely irritated and may ulcerate or become infected. The consequences of this phenomenon can be very detrimental to the health of the eye
Patients with facial paralysis will experience eye irritation, tearing, foreign body sensation and constant eye pain in severe cases. The symptoms are usually worse in air-conditioned environments or while reading for prolonged periods of time. Because the patient is unable to close his eye completely while sleeping, it will be significantly dry and painful in the morning.
Young patients with facial paralysis will usually experience less severe symptoms because they have a healthier tear film that protects the surface of the cornea. On the other hand, older patients and those with preexisting dry eye will experience severe corneal dryness and debilitating symptoms. Patients with glaucoma who use drops to lower eye pressure are also at greater risk for intense eye irritation and corneal ulceration.
Some cases of facial paralysis are temporary and will resolve without treatment in about 6 months. Other cases are permanent and will require physical therapy to improve muscle movement and the symptoms of dry eye. Frequent eye lubrication with preservative-free artificial tears and ophthalmic ointments are essential to keeping the cornea moist and preventing excessive dryness. It is important to protect the eye at night by using an eye patch or moisture chamber glasses. If the eye becomes severely irritated, the patient must see an ophthalmologist to rule out infection, in which case the physician will prescribe topical antibiotic drops. It is also important to avoid the use of air-conditioning. If the symptoms cannot be controlled with topical medications, the patient will need a surgical procedure to restore normal eyelid function.
In cases of irreversible damage to the facial nerve or when there is no improvement with physical therapy, surgical intervention will be needed to help the patient close the eye. The best surgical option is the use of a gold weight implant to restore the blinking mechanism. These implants are biocompatible and do not have to be replaced. The implant works by adding weight to the eyelid and allowing it to close with each blink. This is most important during sleep. An advantage of gold weight implants is that they do not prevent the patient from raising the eyelid. That is, the eye will open and close normally with each blink.
Gold weight implant procedures are done as an outpatient surgery with local anesthesia and mild sedation. The operation is painless and takes about 35 minutes. Swelling and bruising after the surgery are normal but subside in about one week. The patient must avoid lifting heavy objects and exercising for one to two weeks.
Our oculoplastic surgeon is trained in the latest surgical techniques for protection of the eye in facial nerve paralysis. He can help you alleviate your symptoms and prevent sight-threatening complications. Do not hesitate to contact us for a complete evaluation and treatment plan that is suited for you.
Before
After


+506 7032-5570
Abraham Gómez, MD
Hospital Clínica Bíblica, Omega Building, 2nd floor
Loras Medical, Torre Las Loras, main floor
ARTE FACIAL
ARTE FACIAL
Visit us at our new office! 25% off on your consultation at Loras Medical. Book here (Valid Until December 15, 2023.)
Please fill out the form below to schedule a virtual consultation with Dr. Gomez.