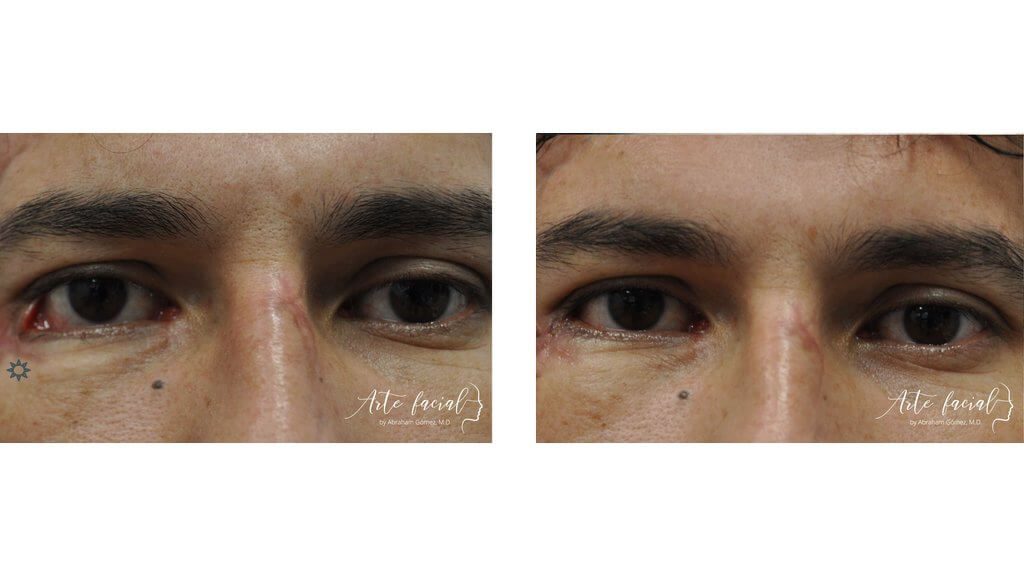
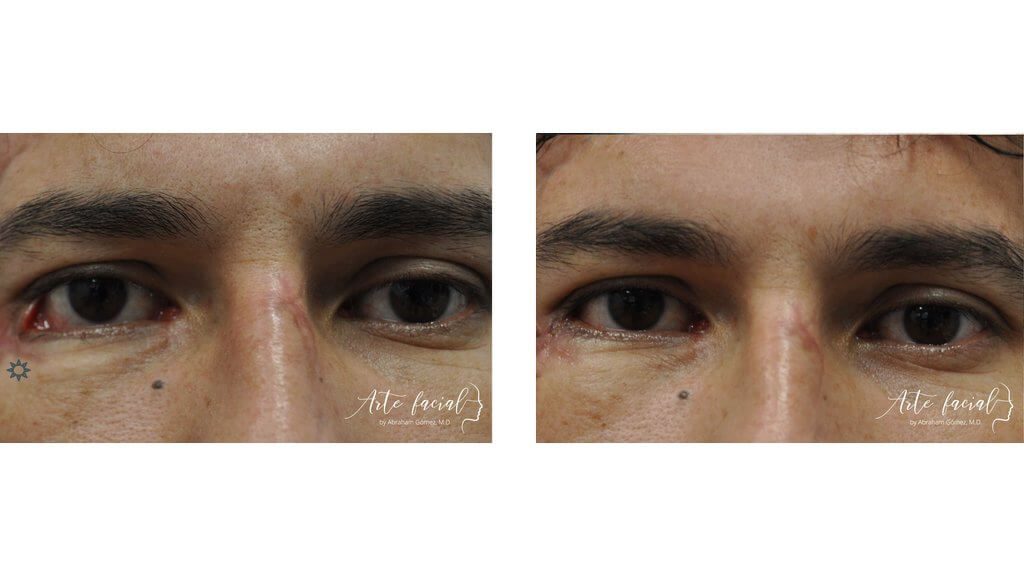
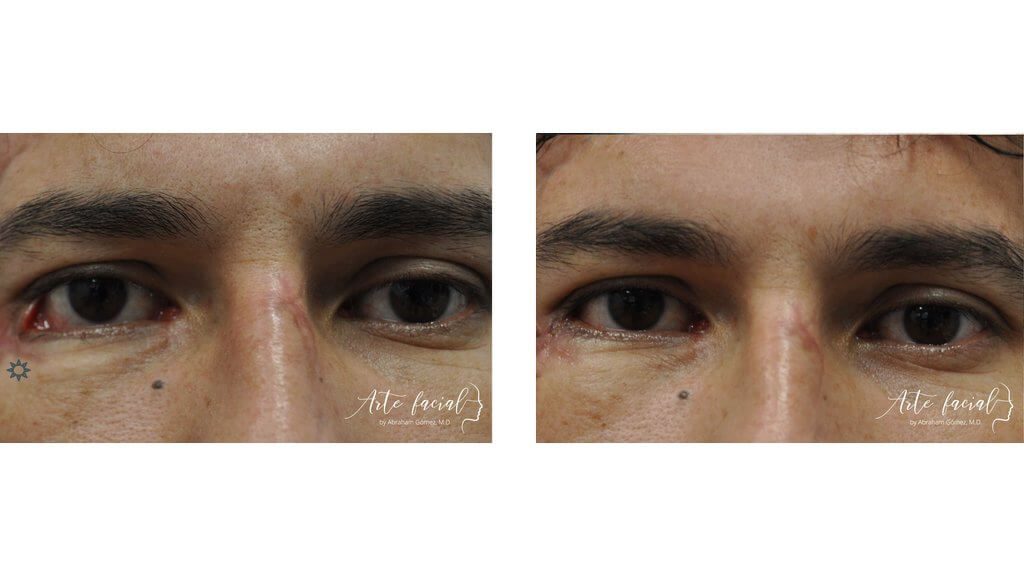
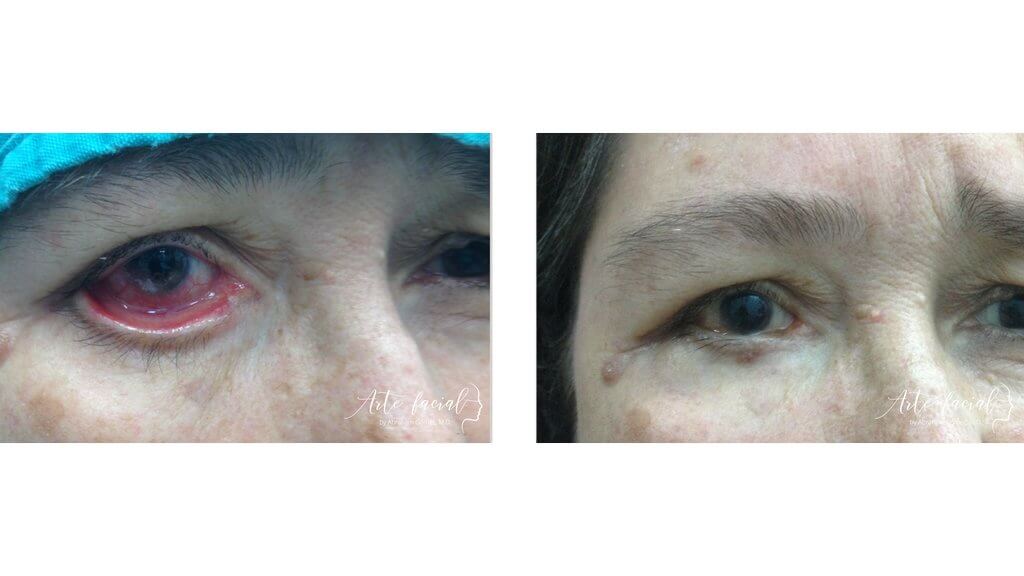
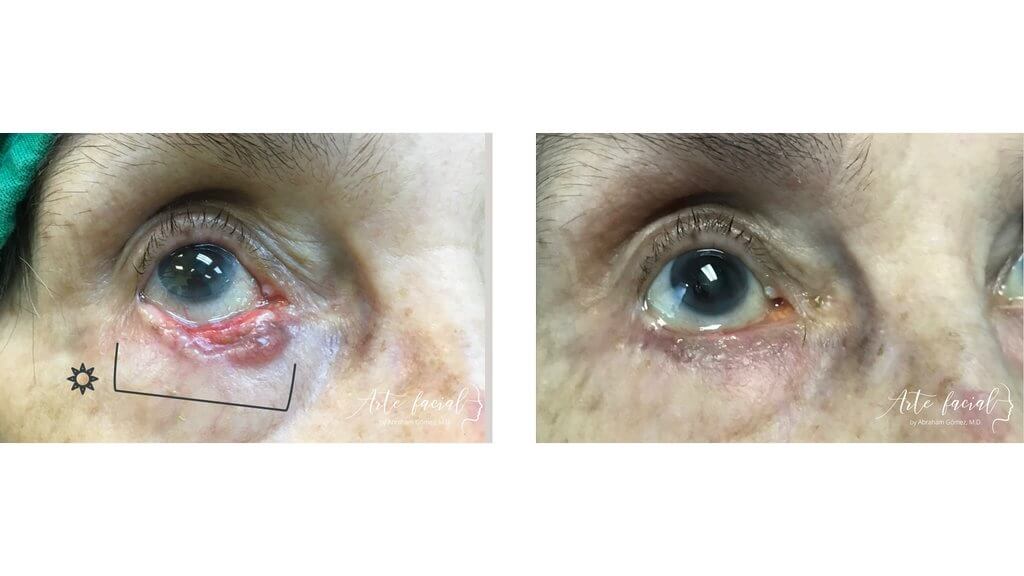
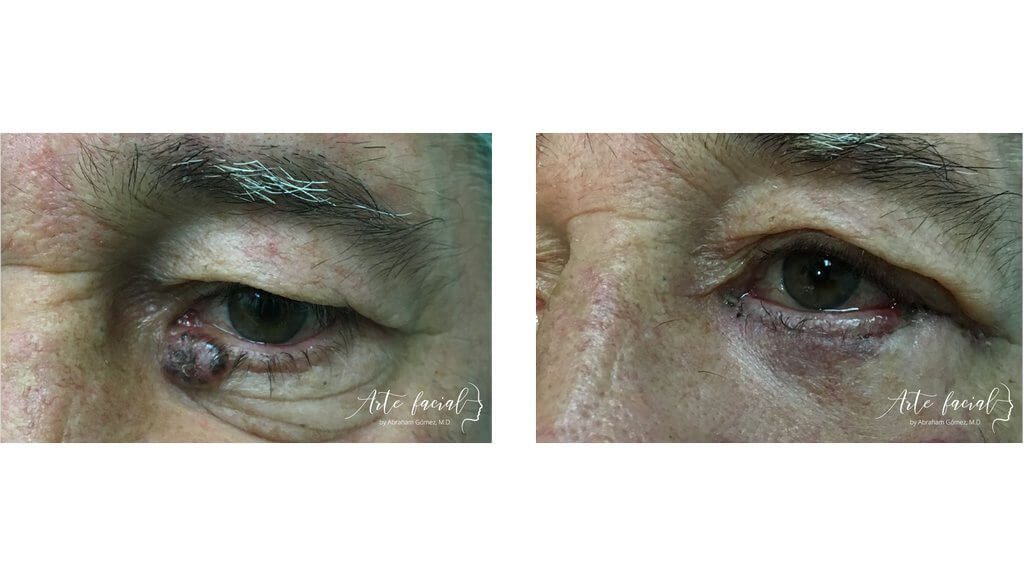
Before
After

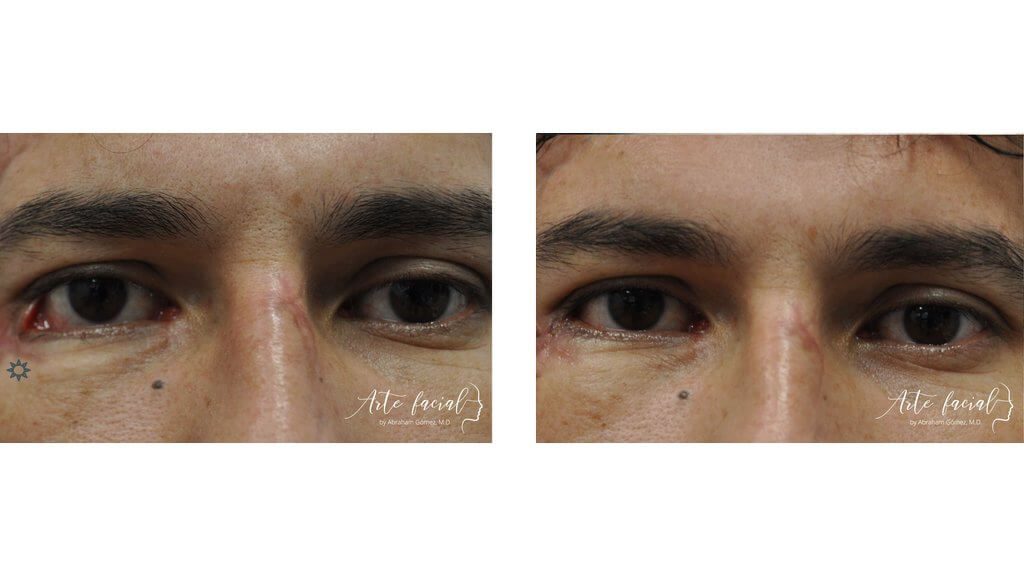
Functional & reconstructive (3)
Functional & reconstructive (4)
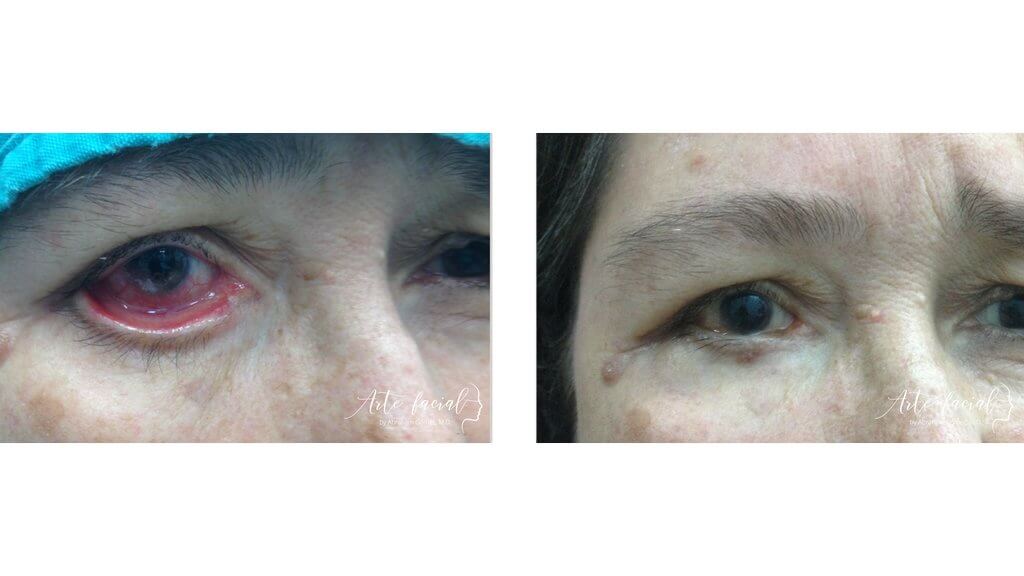
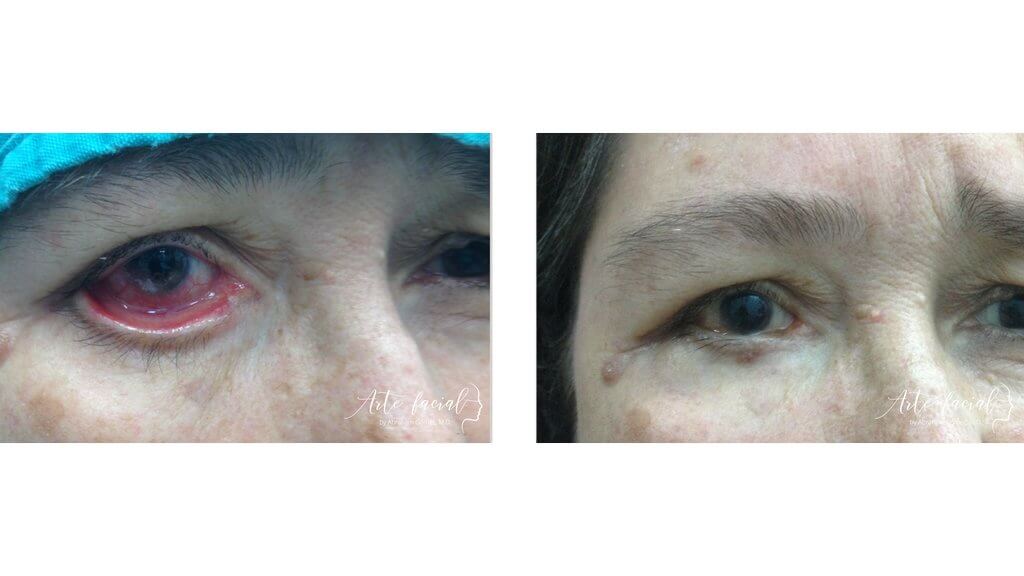
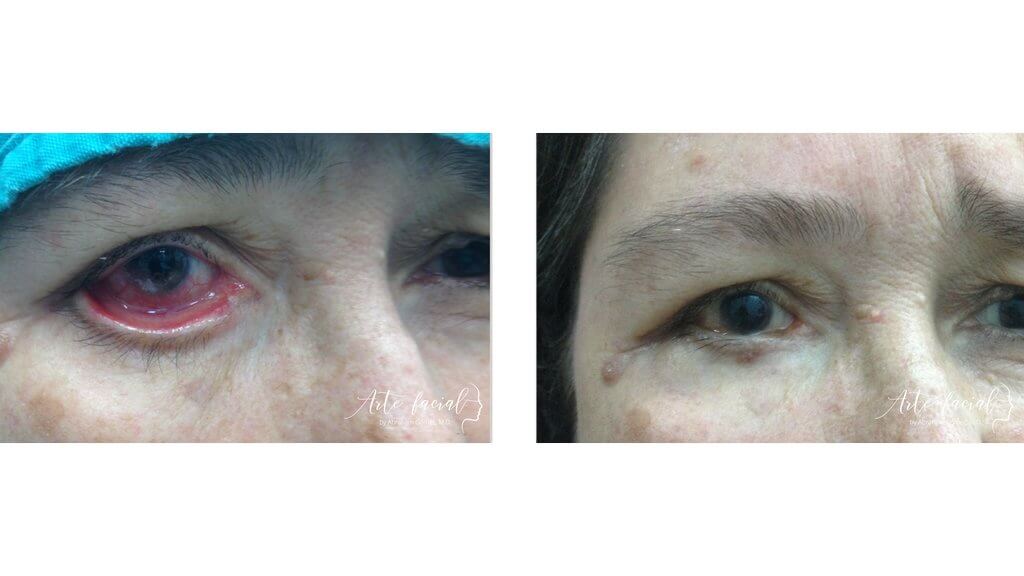
Functional & reconstructive (5)
Functional & reconstructive (6)
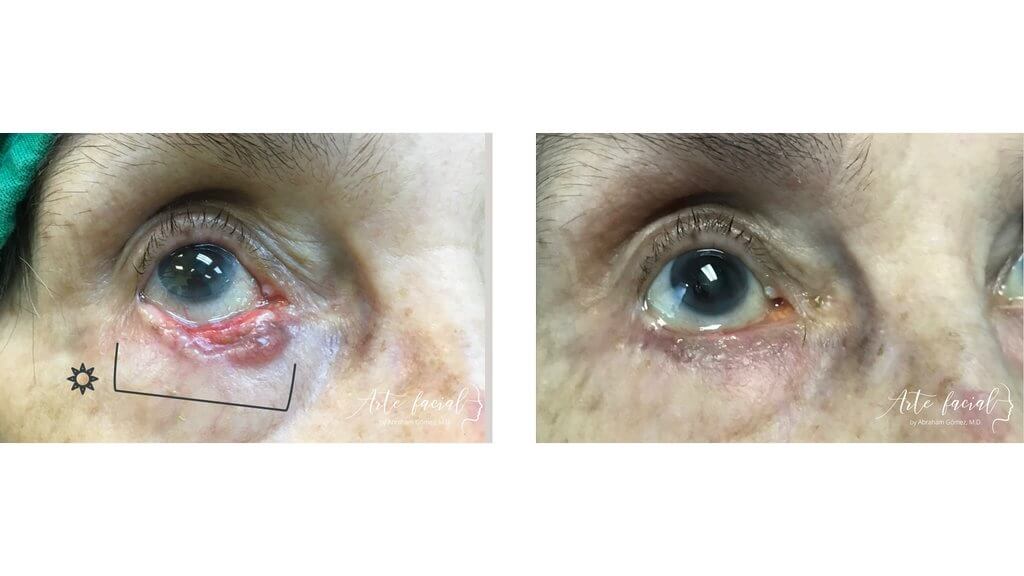
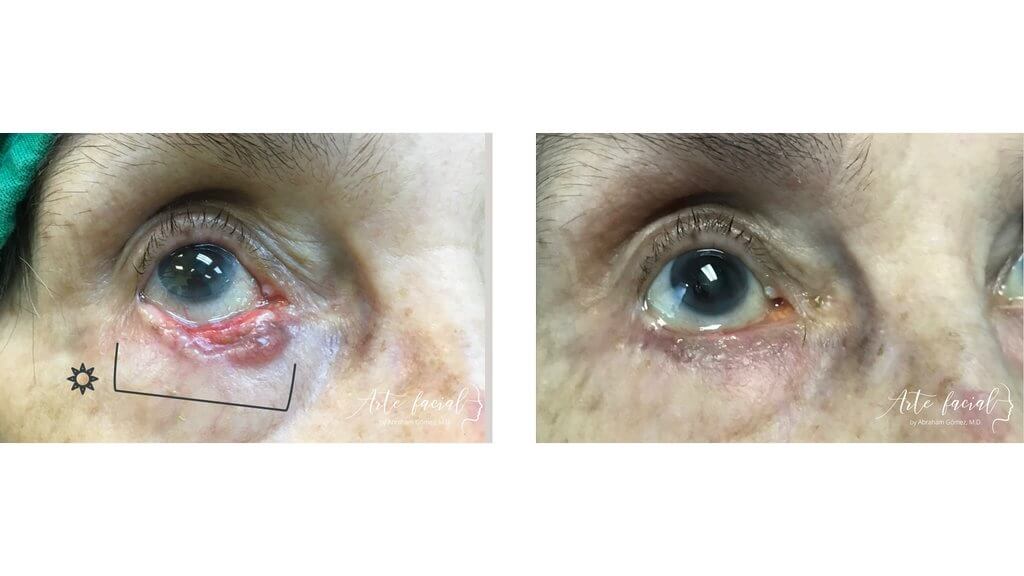
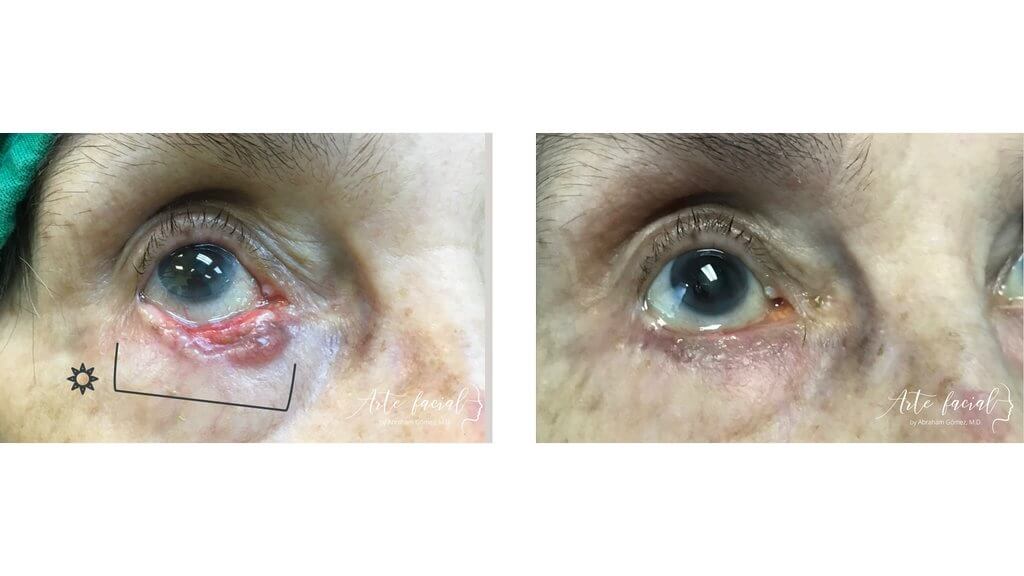
Functional & reconstructive (7)

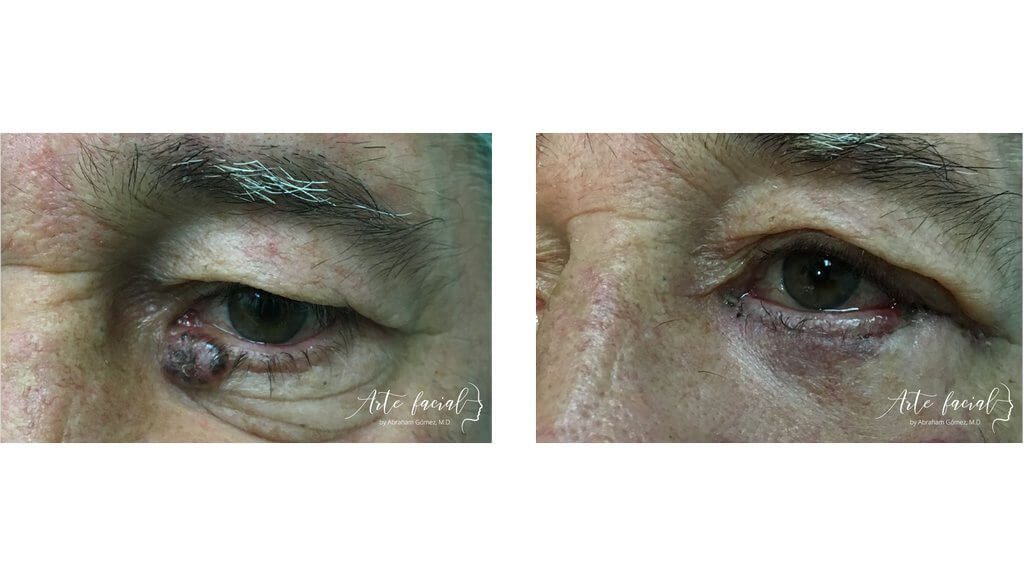
Skin cancer is one of the most common cancers, especially among populations with fair skin, and the eyelid is a frequent target. In fact, up to 10 percent of all skin cancers form on the eyelids, and most appear on the lower eyelid. This condition occurs more frequently in adults between the age of 50 and 80, and rarely affects children and young adults.
Eyelid skin cancer is divided into two categories: melanoma and non-melanoma skin cancer (NMSC). Non-melanoma types are much more prevalent affecting millions of people every year.
A significant positive aspect of skin cancer is that it can be detected early, especially on the eyelids. This makes it much easier to treat and cure. The most common symptom of skin cancer is a mass on the eyelid skin. The skin may take on an unusual appearance, color or texture. The patient may also notice some thickening or scaling of the skin. Bleeding from the mass or a mass that does not heal completely may also indicate malignancy. Loss of eyelashes is a very strong indicator of eyelid cancer, while irregular borders and growth of the lesion indicate probable active growth of the mass.
As mentioned above, eyelid skin cancer falls into two categories: melanoma and NMSC. The eyelids are a common site for the two most frequent types of NMSC: basal cell carcinoma and squamous cell carcinoma.
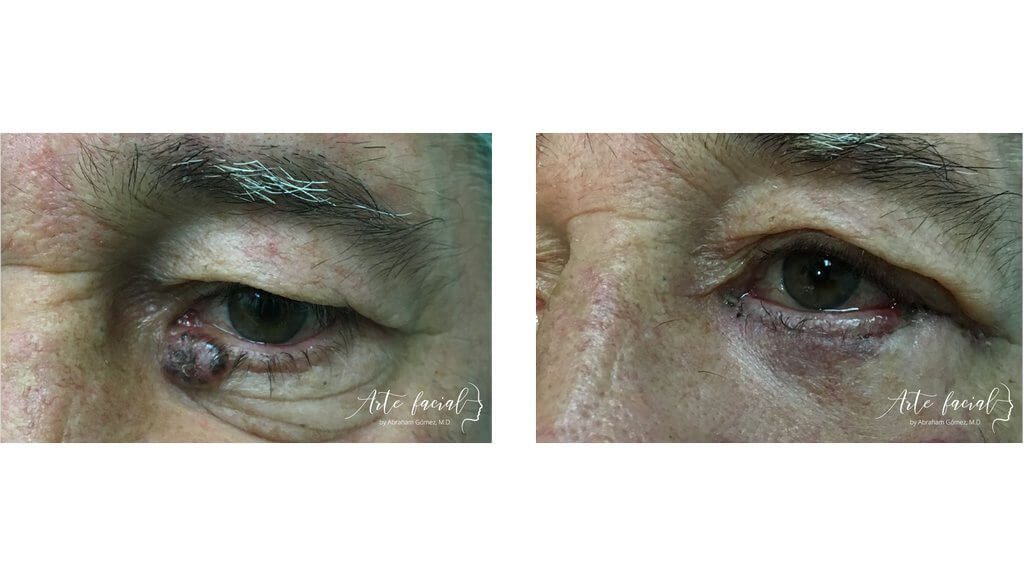
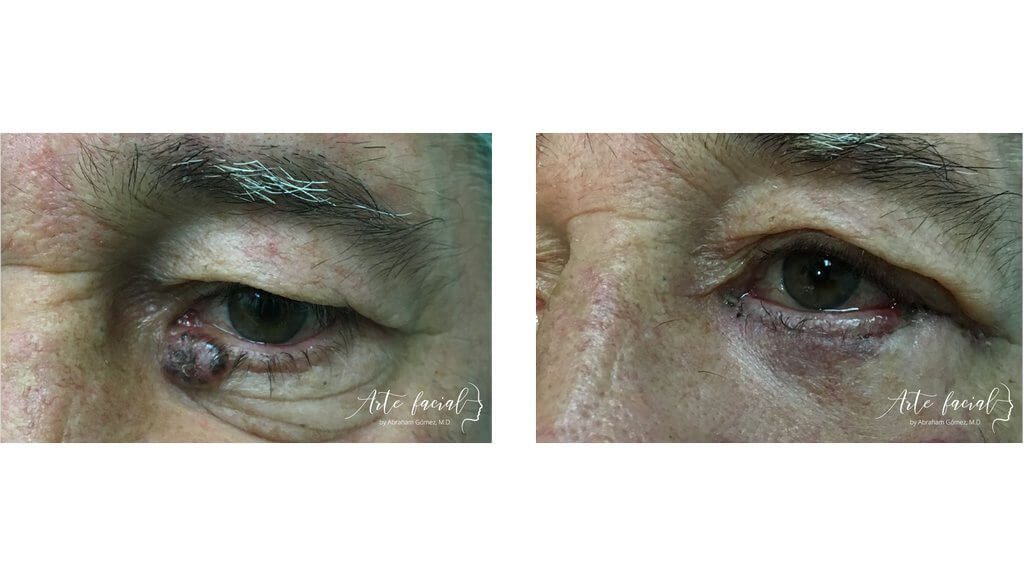
Arises from basal cells which are found in the lower layer of the epidermis. Basal cell carcinomas make up about 90% of all cancers that appear on the eyelids. This cancer carries an excellent prognosis as it does not tend to metastasize; this means that the tumor produces local damage but will rarely travel to other organs. However, the tumor will produce significant local tissue damage if it is not removed promptly. Basal cell carcinoma appears as a “pearly” bump on the eyelid with a scaly surface. The mass grows slowly and does not go away with topical treatments.
A simple clinical examination may suspect basal cell carcinomas; however, the only sure way to make a diagnosis is to biopsy the mass. If in fact the mass is BCC, the surgeon will have to remove it completely. If diagnosed early, the cancer can be removed without leaving any impairment of eyelid function. On the other hand, if the mass has been present for a long time and tissue damage is extensive, the eyelid defect after cancer removal will be significant, and complex eyelid reconstruction will be necessary.
Is the second most common cancer of the eyelids. It is also more aggressive than BCC. Squamous cell cancer arises from a more superficial layer of the epidermis, and although it resembles BCC clinically, the mass is usually flatter and produces more inflammation. A common form of SCC is a red, scaly patch that grows and does not heal. SCC has a poorer prognosis because it spreads to the deeper tissues of the orbit (eye socket) and has a higher tendency to produce metastasis.
is the most aggressive type of eyelid cancer. It usually surfaces as a pigmented mole on the margin of the lid. The pigment is dark brown to black and the borders of the mass are poorly defined. Because this cancer has such a bad prognosis, any pigmented tumor on the eyelid margin should be biopsied.
Once a diagnosis of eyelid skin cancer has been made with a biopsy, the mass must be surgically removed and the area reconstructed. Removing the cancer is most important and no malignant cells should be left behind. There are three surgical techniques to accomplish this: excisional biopsy with wide margins, intraoperative frozen section technique, and Mohs surgery.
Excisional biopsy of the lesion leaving wide margins on the border of the tumor is a popular technique of skin cancer treatment. The visible margins of the tumor are marked with ink and a 3 to 6-mm rim of healthy looking tissue is left around this area. The tumor is removed along with the rim. The advantage of this technique is that it is quickly performed and does not require expensive equipment. The biggest disadvantage is that, even though the tumor is excised, malignant cells may still be present in the margins left behind, and the surgeon will have to go back to remove more tissue from that area.
Frozen section intraoperative biopsy is a technique that consists of removing the area that seems to be affected and sending the specimen to pathology. A surgical pen is used to identify the visible and/or palpable outer limits of the tumor with an additional 3 to 5-mm border marked beyond this. The tumor is then excised at the marked borders. The margin is divided into small units that are sent to a pathologist for examination under a microscope. If the margins are infiltrated, the surgeon returns and removes more tissue which the pathologist analyzes again. This is repeated until the skin margins are completely free of malignant cells.
Mohs surgery is considered the most precise and effective technique to treat non-melanocytic skin cancer. The technique consists of removing layers of skin that are affected by cancer and immediately examining them until only healthy skin remains. It would be like peeling off the layers of a rotten onion until only the good part is left. Mohs technique has the huge advantage of preserving the most quantity of healthy tissue of all three techniques mentioned. The disadvantage lies in the fact that the surgery time can be quite long, even hours, and this requires long sedation. It is also a very expensive technique due to its technical complexity. The eyelid area is particularly amenable to this technique. The reconstruction is not always done the same day of surgery; instead, the Mohs surgeon removes the lesion and the reconstructive plastic surgeon reconstructs one or two days after.
Recovery after eyelid cancer surgery requires that the patient take some time off work to allow tissues to heal properly. The first week the patient should refrain from lifting heavy objects. Swelling and bruising are normal after the surgery and swelling may last a long time if the small lymphatic vessels are damaged. The resulting swelling is called lymphedema and it is quite difficult to treat. Lymphatic drainage therapy can help to reduce this swelling. Some patients may require more than one surgery to recover normal eyelid function.
Cancerous tumors on the eyelids have certain characteristics that distinguish them from benign lesions. You can suspect that you have eyelid cancer if you notice a mass or bump around the eye that does not go away with topical treatments. If the mass has shown signs of growth and bleeds with minor trauma, the probability of cancer is even higher.
Other signs of malignancy are irregular borders, skin ulceration, and loss of eyelashes in the location of the growth. A red, scaly patch on the skin that becomes chronic also raises the suspicion of cancer. The most common form of eyelid skin cancer, called basal cell carcinoma, presents as a growth that has raised, pearly borders and small blood vessels on its base.
These are clinical signs of skin cancer. However, the only way to be certain that a mass is cancer is by taking a biopsy. The pathologist can analyze the specimen and make the diagnosis. This is also critical to know which type of cancer the patient has.
Skin cancer is very common, especially in the face. Eyelid skin cancer is no exception. In fact, this area is responsible for 5 to 10 percent of all skin cancers. Skin cancer is more common in the lower eyelid followed by the medial eyelid, upper eyelid and lateral angle or commissure, in that order.
The most common type of skin cancer is Basal Cell Carcinoma (BCC). This tumor grows from abnormal cells in the deeper layers of the skin. BCC causes local tissue damage but very rarely causes metastasis. This makes BCC one of the most “benign” types of cancer. In fact, most these tumors can be cured surgically and will not require chemotherapy or radiation.
The symptoms of eyelid skin cancer will depend on the type of cancer. Itchy or irritated skin is common in most types. Some people experience pain, although it tends to be mild in most cases. Bleeding from the mass is somewhat uncommon but very characteristic of malignancy. Also, most cancers produce loss of eyelashes, so this symptom should prompt a person to consult an eyelid surgeon quickly.
It is normal to be concerned if you are diagnosed with eyelid cancer. Fortunately, though, most types of cancer in this area have a very good prognosis. The main reason is that these neoplasms rarely cause metastasis. Another reason is that they can be cured with surgery alone and will not require chemotherapy or radiation in most cases. For example, survival rates with Basal Cell Carcinoma (the most common type) are the highest among cancer victims.
On the other hand, malignant melanoma (MM) has a very poor prognosis. This is probably one of the most aggressive types of cancer. Melanoma of the eyelid is covered in a different section of this website.
Treatment of eyelid skin cancer is always surgical. After the diagnosis is made with a biopsy, the cancer is removed very carefully to make sure that no malignant cells are left behind. There are different techniques to accomplish this. The most efficient is called Mohs micrographic surgery. Mohs surgery has revolutionized skin cancer treatment because it allows surgeons to remove the cancer completely while conserving healthy tissue around the tumor. This makes reconstruction of the anatomical site much easier and the result more aesthetic.
Before
After


+506 7032-5570
Abraham Gómez, MD
Hospital Clínica Bíblica, Omega Building, 2nd floor
Loras Medical, Torre Las Loras, main floor
ARTE FACIAL
ARTE FACIAL
Visit us at our new office! 25% off on your consultation at Loras Medical. Book here (Valid Until December 15, 2023.)
Please fill out the form below to schedule a virtual consultation with Dr. Gomez.